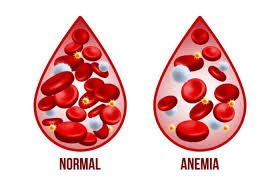
Anemia
Anemia is a condition where the blood has a reduced number of red blood cells or hemoglobin.
It leads to decreased oxygen-carrying capacity, causing fatigue, weakness, and shortness of breath.
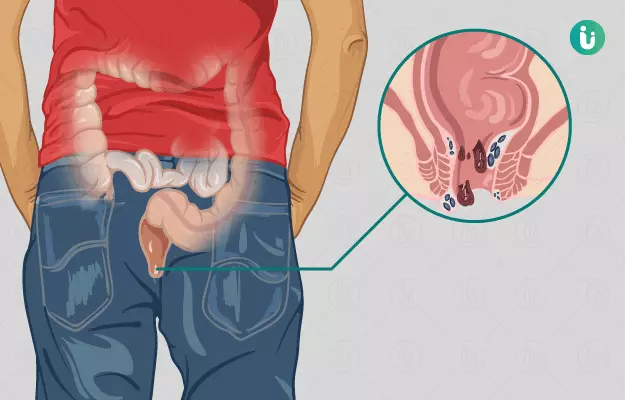
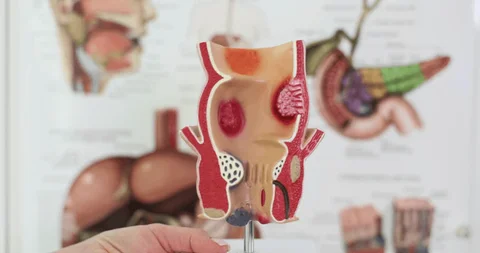
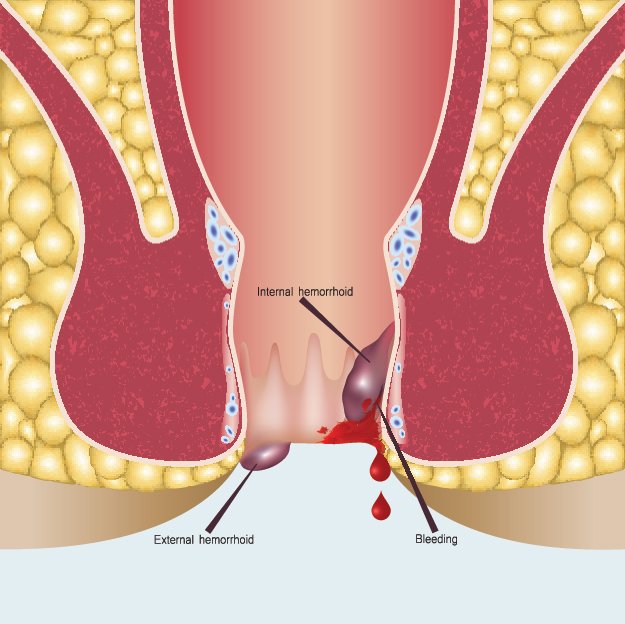
Common causes include nutritional deficiencies (iron, vitamin B12, folate), chronic diseases, or blood loss.
Symptoms may also include pale skin, dizziness, headaches, and rapid heartbeat.
Management depends on the cause and may involve dietary supplements, medications, or treating underlying conditions.